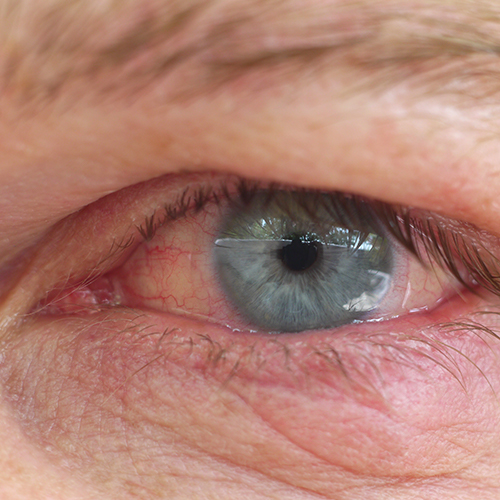
Dry eye disease is considered a common multifactorial (determined by several concomitant factors) tear film disease affecting the ocular surface and caused by reduced tear production and/or increased tear film evaporation.
The condition manifests itself with a wide variety of signs and symptoms, including a decrease in visual function, which significantly affects quality of life.
From an epidemiological point of view, dry eye disease affects between 5% and 50% of the general population. It is more common in women, especially during the menopause, and its prevalence increases with age, affecting between 20% and 30% of people over 50. However, recent studies show that more and more children and adolescents are suffering from this condition, probably due to the prolonged use of electronic devices in play and study.
Dry eye disease is triggered by a number of intrinsic (body-related) and extrinsic (environment- or lifestyle-related) factors including age, gender, levels of certain hormones, autoimmune diseases, climate, smog, smoking, prolonged use of contact lenses and/or electronic devices, and exposure to certain medications.
Despite a better understanding of the mechanism of occurrence of dry eye disease, diagnosis is often not straightforward and treatment is not very effective.


In most cases of dry eye disease, treatment involves the administration of eye drops or gels, known as “artificial tears”, to increase the hydration and lubrication of the eye surface.
Most artificial tears on the market contain hyaluronic acid as their main ingredient: a molecule of natural origin that has important lubricating and moisturising properties. Several other products contain instead carboxymethylcellulose and polyethylene glycol (PEG).
The biggest limitation of these traditional artificial tears is that they act by relieving the symptoms, but do not correct the underlying mechanism that caused them, i.e. the inflammatory state.
In order to address this important factor as well, a new tear substitute has recently been launched on the market which, in addition to hyaluronic acid, contains a very low concentration of hydrocortisone, an active ingredient with anti-inflammatory activity that is the synthetic analogue of cortisol produced by the body. The product therefore has the advantage not only of lubricating and moisturising the ocular surface, but also of controlling the inflammatory component. Indeed, by replenishing endogenous cortisol, no longer produced by the system in crisis, it helps restore homeostasis.
In the most severe dry eye conditions, when the inflammation has become evident and the condition is now chronic, treatment may involve the use of actual courses of steroid drugs or cyclosporine, which should be prescribed by a specialist and used under strict medical observation. Artificial tears should always be included at any stage of the disease: they should not be recommended but prescribed, they should be used regularly and not only when needed, carefully following the instructions of the ophthalmologist. In addition, it is preferable to choose a preservative-free formulation, as preservatives may aggravate the already compromised condition of the ocular surface.
Dry eye disease must therefore be recognised as early as possible and treated appropriately by acting simultaneously on all the components that support and contribute to it.
It is now clear that dry eye disease is established and maintained by the loss of the ocular surface’s ability to maintain its balance (homeostasis) by responding and adapting to the many harmful external or internal stimuli to which it is exposed.
As long as the insult is mild or short-lived, the ocular surface can compensate for the loss of homeostasis through the physiological mechanism of para-inflammation or sub-clinical inflammation (i.e. a non-noticeable inflammatory state). But what regulates para-inflammation? It seems that the protagonist is cortisol produced by the ocular surface itself, which in small quantities is able to cope with the insults and damaging stimuli to which our eyes are exposed on a daily basis (wind, dry air, dust, etc.). But if the damaging stimulus becomes intense or continuous and persistent, cortisol synthesis is blocked, the system stops working and the para-inflammation that is no longer controlled degenerates into chronic inflammation that triggers the disease with severe signs and symptoms.





How do you rate your experience on our site?
Comments
You need to log in to post a comment
No comments inserted